Environmental harm is no longer a distant concern; it is a direct threat to health outcomes worldwide. Yet, many health systems continue to ignore their environmental footprint. Hospitals, clinics, and labs produce waste, use energy-intensive equipment, and sometimes expose nearby communities to harmful chemicals.
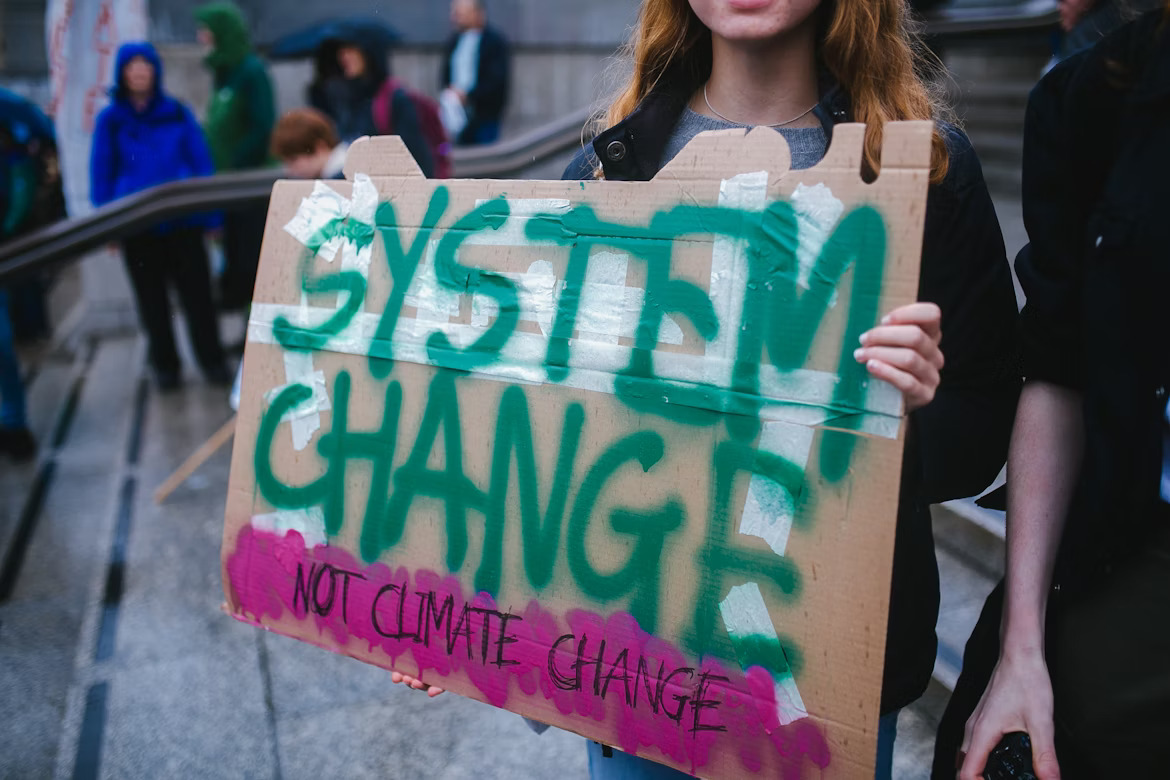
While healthcare focuses on saving lives, it often overlooks the environments that sustain life. The need for change is urgent. An effective environmental strategy should be built into every level of healthcare.
This article aims to explore why environmental responsibility must become a healthcare priority.
The Connection Between Climate and Chronic Illness
Chronic illnesses such as asthma, heart disease, and respiratory disorders are rising across the globe. Environmental factors are a major cause. Air pollution, rising temperatures, and unsafe water sources are worsening these conditions. Healthcare systems must begin to treat environmental health as part of preventive care.
The 2023 Lancet Countdown reports that adults over 65 now experience twice as many annual heatwave days compared to the period from 1986 to 2005. Infants and seniors are highly vulnerable to heat-related illnesses, heart conditions, and respiratory distress from worsening air pollution.
Droughts and floods are severely damaging food systems, driving malnutrition and increasing chronic diseases like diabetes and hypertension. In 2021, 127 million more people faced serious food insecurity than global averages from previous years.
This rise deepens the link between climate change and chronic illness, especially in vulnerable or under-resourced communities. 27% of surveyed cities now fear their health systems may collapse due to climate-driven medical demands.
Health systems can address this through clean-energy operations, sustainable designs, and climate-aware clinical care models. Promoting green infrastructure helps reduce disease.
How Poor Planning Puts Communities in Danger
As cities grow, fast expansion often takes priority over proper planning, putting communities at long-term health risks. Poorly designed infrastructure increases exposure to air pollution, flooding, and extreme temperatures, especially in underserved neighborhoods. Many growing cities lack clean water, effective waste disposal, and safe housing, leaving vulnerable groups without protection.
According to a 2023 study in ResearchGate, rapid urbanization in developing countries is reshaping health outcomes for billions. Most city residents breathe unhealthy air and face poor sanitation, limited healthcare access, and unsafe transportation systems. These conditions raise the risks of chronic illnesses, infectious outbreaks, and preventable deaths in low-income urban areas.
Pollution sources within cities, including healthcare-related activities, also worsen environmental damage when left unchecked or poorly managed. Some medical sterilization companies use harmful chemicals that can severely affect the surrounding community if emissions are unregulated.
One notable example is Sterigenics, a sterilization company that reportedly emitted high levels of ethylene oxide from its Atlanta facility for years. Investigations revealed that emissions from the Sterigenics Atlanta facility exposed nearby residents and plant workers to toxic levels of the gas. This happened without their knowledge, greatly increasing their risk of cancer and other serious illnesses.
According to TorHoerman Law, victims are collaborating with legal teams to seek justice for the physical, financial, and emotional toll suffered. This case highlights how poor planning and weak oversight can deeply harm the very communities that systems are meant to protect.
The Consequences of Negligence
The healthcare industry plays a vital role in saving lives, but negligence within the system can have unintended consequences. Operational carelessness, outdated technologies, and a lack of sustainability planning can silently worsen both public health and environmental conditions.
According to research from Harvard, the global healthcare sector is responsible for roughly 4.4 to 5.2% of all greenhouse gas emissions. These emissions drive climate change while indirectly increasing respiratory illnesses, cardiovascular problems, and other chronic health conditions.
Without accountability, hospitals and clinics risk becoming part of the problem they are designed to solve. For instance, excessive energy use, improper waste disposal, and inefficient resource management all contribute to a harmful ecological footprint. Over time, such practices harm vulnerable populations the most.
Policies That Can Future-Proof Healthcare Delivery
The future of healthcare depends on strong, enforceable policies that prioritize environmental responsibility. Without clear rules, even well-meaning institutions fall short. Systems need policies that cover energy use, waste handling, and environmental impact from the ground up.
To future-proof healthcare, global networks like Global Green and Healthy Hospitals (GGHH) are leading efforts to embed sustainability into policy and practice. In 2023, over 280 new institutions joined GGHH, reflecting a growing commitment to climate-smart healthcare. Initiatives like the Climate Impact Checkup and the Healthcare Climate Challenge help institutions assess their climate footprint and set measurable goals.
Notably, 85% of Challenge participants have adopted formal policies focused on climate mitigation and resilience. These collective actions signal a shift toward healthcare systems that are both environmentally responsible and prepared for future climate-related disruptions.
Health facilities must follow these models to build resilience. Adopting clean energy, reducing plastics, and monitoring air quality are essential steps. These efforts reduce environmental harm while saving long-term operational costs. Hospitals also build public trust by leading in environmental care.
Frequently Asked Questions:
1. Why should hospitals care about environmental strategy?
Hospitals impact the environment through waste, energy, and emissions. An effective strategy lowers harm, boosts efficiency, and builds public trust. It also supports long-term health goals by reducing pollution-related illnesses and aligning medical care with broader community well-being.
2. How does environmental strategy relate to preventive healthcare?
Environmental factors drive many chronic and infectious diseases. Clean air, safe water, and sustainable operations reduce health risks. By prioritizing environmental strategy, hospitals actively support preventive care and reduce disease burden, especially in vulnerable populations affected by pollution and climate-related threats.
3. What risks do hospitals face by ignoring environmental responsibility?
Hospitals that ignore environmental issues risk legal trouble, fines, and community backlash. Regulatory agencies are tightening standards. Poor practices can cause real harm, making institutions liable for damages and losing public confidence. This may affect funding and long-term operations.
The environmental impact of healthcare systems is shaping the health of entire communities. Strong policies, smart planning, and climate awareness must guide every step. Preventing illness begins with protecting the world in which patients live. A healthier planet leads to healthier people.